Abstract
An electrochemical biosensor based on modified carbon screen-printed electrodes was developed for the detection of hemagglutinin of influenza A H1N1 virus (H1). Gold nanoflowers were electrodeposited on the electrode to increase conductivity and surface area. The electrochemical signal was amplified by functionalization of the gold nanoflowers with 4-aminothiophenol, which resulted in a 100-fold decrease of the charge transfer resistance due to a tunneling effect. Subsequently, monoclonal antibodies against H1 were immobilized on the surface via covalent amide bond formation, followed by blocking with bovine serum albumin to minimize nonspecific hydrophobic binding. The electrodes were characterized by cyclic voltammetry and electrochemical impedance spectroscopy experiments in the presence of [Fe(CN)6]3−/4−. Differential pulse voltammetry was used to measure the change in current across the electrode as a function of H1 concentration. This was performed on a series of samples of artificial saliva containing H1 protein in a clinically relevant concentration range. In these experiments, the biosensor showed a limit of detection of 19 pg/mL. Finally, the biosensor platform was coupled to an automated microfluidics system, and no significant decrease of the electrochemical signal was observed.
Introduction
Viral infections pose a threat to medical and public health systems, and the economic expenditures due to viral infections have increased steadily for health care systems in past years [1]. Influenza is an acute respiratory disease in mammals and domestic poultry, which emerges from zoonotic reservoirs in aquatic birds and bats. Influenza viruses are capable of evolving at a fast rate; they have a segmented single-stranded negative-sense RNA genome that is devoid of proofreading systems, resulting in a constant accumulation of mutations in their genome [2]. Influenza viruses belong to the Orthomyxoviridae family and are categorized into four groups, namely, influenza A, B, C, and D viruses. The antigenic features of the hemagglutinin (HA) and neuraminidase (NA) glycoproteins on the surface of influenza A viruses are used to further classify the virus into subtypes. Influenza A comprises 18 HA subtypes and 11 NA subtypes, of which only the H1, H2, H3, N1 and N2 strains have been associated with widespread human epidemics [3]. H1 protein initiates infection by binding to the cell surface and inducing membrane fusion. This protein is considered as a prime determinant of the pathogenicity and is the most abundant influenza surface glycoprotein [4]. These features make H1 protein a great target for biosensing.
Traditionally, infections caused by influenza A H1N1 are diagnosed through viral culture, immunofluorescence assay, and enzyme-linked immunosorbent assay (ELISA) [5]. These techniques suffer from two key drawbacks. They require lengthy protocols that take a few days to complete, and they fail to detect the virus at early stages of infection because of the low concentration of viral particles. However, detection of viral infections at early stages of infection is essential to prevent the dissemination of pathogens and the emergence of future pandemics.
Recently, molecular methods capable of detecting viral pathogens have gained more attention because of their inherent high sensitivity and specificity compared to conventional methods. Among these methods, nucleic acid amplification assays such as reverse transcriptase polymerase chain reaction and loop‐mediated isothermal amplification assays have shown great sensitivity for the detection of influenza A virus. These techniques target the genetic material of the virus, and meticulous protocols are required to perform the extraction from the samples [5]. Moreover, they require highly specialized infrastructure built in place as well as trained professionals, making detection methods based on nucleic acid detection and amplification less accessible [6].
Rapid, sensitive, reliable, and easily available diagnostic methods for influenza A H1N1 virus are needed to detect infected patients at an early stage to improve treatment options, recovery time, and economic cost. Biosensors are widely used to detect and quantify different analytes. They incorporate a biorecognition element for detection of the analyte of interest in a sample and a physicochemical transducer to generate measurable signals that reflect the concentration of the analyte [7]. Among different types of biosensors, electrochemical biosensors are particularly advantageous, since they can be built from low-cost components, designed to be compact and portable, while preserving high resolution, accuracy, and sensitivity [8].
In the last few years, various biosensors for the detection of influenza A H1N1 virus have been developed. Detection of influenza A H1N1 virus can be achieved by targeting one or more relevant biomolecules of the virus. The majority of studies have targeted H1 protein [9-20], while others have focused on N1 protein [8,21], both H1 and N1 proteins [22], nucleoprotein [23-25], both H1 and nucleoprotein [26], nucleic acids [27-29], matrix protein [30], and serum amyloid A biomarker [31]. Biosensing technologies are constantly improved; the challenge is to create portable devices that overcome drawbacks related to long incubation times, unsatisfactory limits of detection, low stability, and short shelf life of the biosensor.
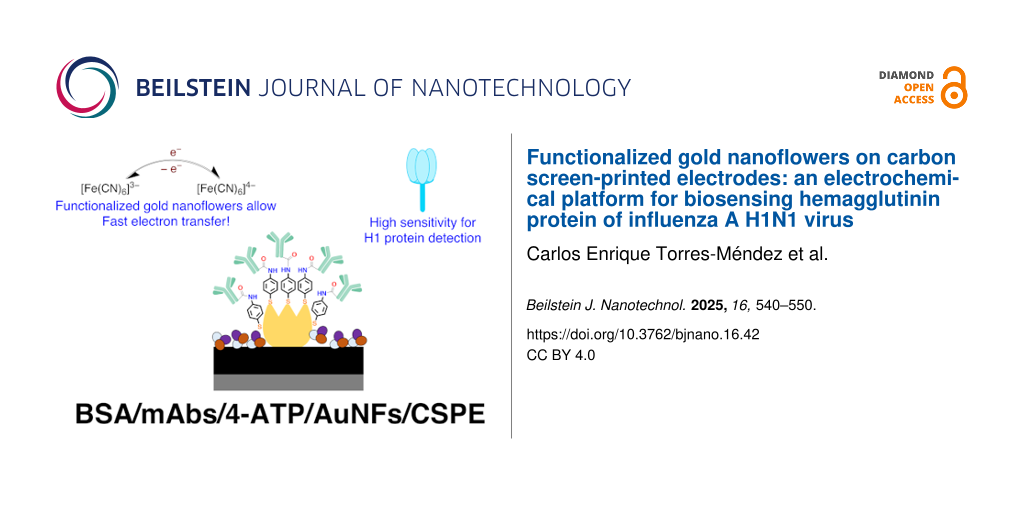
To address the current challenges, in this study, we built an electrochemical biosensor to detect and quantify H1 of influenza A H1N1 virus at clinically relevant concentrations with high accuracy and sensitivity in a complex matrix such as artificial saliva (Figure 1). The biosensing system can also be coupled to a microfluidics system without significant decrease in the electrochemical response. The transducer system of our biosensor is based on low-cost carbon screen printed electrodes (CSPEs) modified with functionalized gold nanoflowers (AuNFs). The complex morphology and surface functionalization of the nanoparticles with 4-aminothiophenol (4-ATP) significantly increased the surface area and the electron charge transfer at the surface of the electrode. To the best of our knowledge, this is the first time that the charge transfer enhancement with 4-ATP, a small organic molecule with delocalized π-electron system, has been employed to improve the sensitivity of electrochemical biosensing of proteins. This approach to amplify the electrochemical signal for biosensing of H1 provides a platform for the early detection of influenza A H1N1 virus.
![[2190-4286-16-42-1]](/bjnano/content/figures/2190-4286-16-42-1.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 1: Preparation of the biosensing system and the effect on electrochemical current upon H1 protein recognition.
Figure 1: Preparation of the biosensing system and the effect on electrochemical current upon H1 protein reco...
Results and Discussion
In this study, an electrochemical biosensor exhibiting enhanced electron charge transfer properties was constructed in order to detect the presence of the well-known biomarker H1 protein of influenza A H1N1 virus. This biosensor employs a differential pulse voltammetry technique to quantify H1 protein. The developed biosensor combines commercial electrodes with functionalized nanostructures and monoclonal antibodies to recognize H1 protein at clinically relevant concentrations.
Scanning electron microscopy
Scanning electron microscopy (SEM) analysis was explored to characterize the surface of the electrodes after electrodeposition of gold nanoparticles (Figure 2). Because of the high conductivity of gold, a difference in contrast is observed when comparing the surface of the commercial CSPE (Figure 2A) to that of the AuNFs/CSPE (Figure 2B). The gold nanoparticles are evenly distributed across the surface of the electrode (Figure 2C). The deposited nanoparticles show a flower-like morphology with an average size of 139 nm and a standard deviation of 44 nm, which suggests size polydispersity (Figure 2D). The flower-like morphology of the nanostructures provides small Au domains across the electrode surface. The shape of these domains confers them with larger surface area than other types of nanostructures with plain geometric forms.
![[2190-4286-16-42-2]](/bjnano/content/figures/2190-4286-16-42-2.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 2: SEM images of (A) CSPE and (B, C) AuNFs/CSPE; (D) size distribution of the gold nanoflowers on AuNFs/CSPE.
Figure 2: SEM images of (A) CSPE and (B, C) AuNFs/CSPE; (D) size distribution of the gold nanoflowers on AuNF...
Electrochemical characterization
Although CSPEs have advantageous features such as low cost and wide availability, they tend to possess a characteristic high electrical resistance due to the use of inks containing organic molecules and polymeric binders during the fabrication process [32]. This could be seen experimentally (black curve of Figure 3), where the cyclic voltammetry (CV) analysis shows a large peak-to-peak separation of 0.72 V for the [Fe(CN)6]3−/4− redox pair. This differs significantly from the theoretical 0.057 V peak-to-peak separation in reversible redox processes that involve one electron [33]. Typically, the sensing capabilities of electrochemical systems can be limited by the effective electroactive area of the electrode [34]. One approach to increase this parameter is the modification of electrodes with nanostructures that possess high surface area [35]. The strategy based on electrodeposition of gold nanoflowers increased the current response of the electrode because of the larger electroactive surface area compared to a CSPE (Figure 3). The CV analysis of the AuNFs/CSPE showed a peak-to-peak separation of 0.37 V. This value is smaller than in the commercial CSPE, which implies that electron transfer at the electrode surface was enhanced, increasing the redox reversibility for the [Fe(CN)6]3−/4− pair. CSPEs are reported to possess a rough surface at the nanoscale [34]. The electrodeposition technique employed takes advantage of this to control the nucleation process, forming stable AuNFs that remain at the surface of the electrode upon contact with water and ethanol as no change in the CV was observed after contact with these solvents (Supporting Information File 1, Figure S1). This suggests strong mechanical adhesion of the AuNFs to the CSPE surface.
![[2190-4286-16-42-3]](/bjnano/content/figures/2190-4286-16-42-3.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 3: CV characterization at different steps of the electrode modification, measurements performed in 0.1 M KCl containing 5 mM [Fe(CN)6]3−/4−. The scan rate was 100 mV/s.
Figure 3: CV characterization at different steps of the electrode modification, measurements performed in 0.1...
The largest change in the CV was observed after the functionalization of the AuNFs with 4-ATP through stable Au–S bonds. In this case, the peak-to-peak separation for the 4-ATP/AuNFs/CSPE was 0.16 V, showing that the redox reversibility for the [Fe(CN)6]3−/4− pair and the current response of the electrode increased. This effect is known as tunneling charge transfer enhancement and significantly improved the sensitivity of the biosensor. It can be attributed to electron transfer through bonds due to the small length (0.59 nm) and the delocalized π-electron system of the 4-ATP linker molecule. Interestingly, the existence of this effect in a material appears to depend on the size of the superficial nanostructures. A similar effect has been reported for 4-ATP-functionalized multilayered nanostructures of Ag, Au, and Pt with a size range between 48 and 130 nm [36,37] as well as for 4-ATP-functionalized nanohybrids of MoSe2−CsPbBr3 with a size range between 60 and 80 nm [38]. This effect has been relevant to enhance the Raman scattering vibrational modes in surface-enhanced Raman spectroscopy measurements. It has also been noticed that the shape of the nanostructure can be used to tune the magnitude of the charge transfer enhancement by a factor of eight according to studies on spheres, tetrapods, cubes, and dogbone nanoparticles [36]. In contrast, no enhancement effect, or even slower charge transfer kinetics have been observed for 4-ATP-functionalized gold nanoparticles bearing sizes between 5 and 25 nm [39-43]. Therefore, the functionalization of the AuNFs with the linker 4-ATP represents one of the outstanding characteristics of our biosensing system. To the best of our knowledge, this is the first time that this enhancement effect has been explored to improve the sensitivity of electrochemical biosensing of proteins.
Covalent oriented immobilization of monoclonal antibodies (mAbs) was achieved through amide bond formation between terminal carboxylate moieties of mAbs and surface amine groups of the 4-ATP/AuNFs/CSPE. Using this strategy, the fragment crystallizable region of the mAbs is the section bound to the surface. This leads to proper antibody orientation such that the entire antigen binding site is available for adequate biorecognition [44]. No significant peak-to-peak separation change was observed in the CV analysis after immobilization of mAbs and blocking with bovine serum albumin (BSA) (Figure 3). This suggests that the final sensing platform preserved the favorable electrochemical properties achieved using AuNFs functionalized with 4-ATP.
Electrochemical impedance spectroscopy (EIS) was performed to study the charge transfer processes at the surface of the modified electrode (Figure 4). In general terms, the elements of an electrochemical biosensor are analogous to the elements of an electric circuit [45]. A Randles equivalent circuit model was found to fit the experimental data obtained from the EIS analysis. This circuit contains a resistor (Rs) to represent the ohmic resistance of the phosphate-buffered saline (PBS) electrolyte solution. The circuit is connected in series to the parallel combination of a capacitor (Cdl) representing the double layer capacitance of the electrode–solution interphase and a resistor (Rct) accounting for the faradaic charge transfer resistance. A modulation of the Rct magnitude was observed after each modification step on the working electrode of the biosensor (Supporting Information File 1, Figures S2–S6). Finally, the circuit is connected in series to a Warburg element (Wz) representing the diffusion of the [Fe(CN)6]3−/4− employed as redox probe in this study.
![[2190-4286-16-42-4]](/bjnano/content/figures/2190-4286-16-42-4.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 4: Electrical impedance spectroscopy measurements at different steps of electrode modification, recorded in 0.1 M KCl containing 5 mM [Fe(CN)6]3−/4−.
Figure 4: Electrical impedance spectroscopy measurements at different steps of electrode modification, record...
The magnitude of the Rct of the electrodes at different modification stages was calculated by fitting the experimental Nyquist plots to the Randles equivalent circuit model. The commercial CSPE showed a high Rct of 12.90 kΩ (Supporting Information File 1, Figure S2). Electrodeposition of AuNFs improved the electrochemical properties of the electrode by decreasing Rct to 2.35 kΩ (Supporting Information File 1, Figure S3). The Rct of the electrodes decreased to 126 Ω after functionalization with 4-ATP (Supporting Information File 1, Figure S4). These results indicated charge transfer enhancement at the surface of the 4-ATP/AuNFs/CSPE. In this system, Rct was decreased by 100 times, a desired feature to improve the sensitivity of a biosensor. Immobilization of mAbs and blocking with BSA increased the Rct to 825 Ω (Supporting Information File 1, Figure S5) and 1278 Ω (Supporting Information File 1, Figure S6), respectively.
The current response of the 4-ATP/AuNFs/CSPE in the presence of the electrochemical probe [Fe(CN)6]3−/4− was studied using cyclic voltammetry at varying scan rates (Figure 5). Both the cathodic and anodic currents showed a linear correlation to the square root of the scan rate (Figure 6), suggesting that the reduction and oxidation of the complex [Fe(CN)6]3−/4− is a diffusion-controlled process.
![[2190-4286-16-42-5]](/bjnano/content/figures/2190-4286-16-42-5.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 5: Cyclic voltammogram of the 4-ATP/AuNFs/CSPE at different scan rates, recorded in 0.1 M KCl containing 5 mM [Fe(CN)6]3−/4−.
Figure 5: Cyclic voltammogram of the 4-ATP/AuNFs/CSPE at different scan rates, recorded in 0.1 M KCl containi...
![[2190-4286-16-42-6]](/bjnano/content/figures/2190-4286-16-42-6.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 6: Linear models for the dependence of the current on the square root of the scan rate for the 4-ATP/AuNFs/CSPE.
Figure 6: Linear models for the dependence of the current on the square root of the scan rate for the 4-ATP/A...
The performance of mouse monoclonal influenza A H1N1 hemagglutinin antibodies was tested using sandwich ELISA. They were selected as biorecognition element in our electrochemical biosensor after confirming the high specificity for hemagglutinin. In the ELISA, the limit of detection (LOD) of the viral H1 protein was determined to be 0.1 ng/mL.
Biosensor response to standard solutions of H1 protein
The biosensor was characterized using known concentrations of H1 protein dispersed in artificial saliva. Clinically relevant concentrations from 10 to 10,000 pg/mL were measured in a differential pulse voltammetry (DPV) experiment. Artificial saliva was used as a negative control to validate detection accuracy. The DPV technique was used for detection and quantification of antigen load because a good signal-to-noise ratio response was observed, making this detection a rapid and accurate process. Under the optimal parameters (pulse amplitude = 86 mV, potential increment = 4 mV, and scan rate = 100 mV/s), the negative control and four different concentrations (10, 100, 1,000 and 10,000 pg/mL) of viral surface protein H1 were measured with an incubation time of 25 min at RT. Experimentally, a significant difference between the generated current of the blank and the solutions containing H1 was observed (Figure 7a). Furthermore, a linear correlation was established between known sample concentration and current change in order to estimate H1 concentration in unknown samples. This correlation has a high R-square value of 0.9979 (Figure 7b).
![[2190-4286-16-42-7]](/bjnano/content/figures/2190-4286-16-42-7.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 7: (a) Differential pulse voltammetry of the BSA/mAbs/4-ATP/AuNFs/CSPE, recorded in 0.1 M KCl containing 5 mM [Fe(CN)6]3−/4− after 25 min exposure to artificial saliva standard solutions of H1 protein. (b) Calibration curve determined as the dependence of the change in current on the logarithm of the H1 protein concentration.
Figure 7: (a) Differential pulse voltammetry of the BSA/mAbs/4-ATP/AuNFs/CSPE, recorded in 0.1 M KCl containi...
Microfluidics system
The final BSA/mAbs/4-ATP/AuNFs/CSPE was assembled with a microfluidics system. Upon exposition to H1 protein and measurement employing the standard DPV experiment (n = 3), a decrease in current response of 3.1% was observed (Figure 8) in comparison to a measurement without the microfluidics system. This decrease was probably due to a slight reduction in the surface area of the working electrode once the biosensor was assembled, sealed, and attached to the microfluidics system. The compatibility of biosensing devices with microfluidics systems is desired as this combination has the potential to miniaturize and shorten the acquisition time required to process a large number of biological samples, for example, in clinical measurements [46]. Furthermore, compatibility with microfluidic devices is important for the development of portable biosensing devices with automated functions and of simple use.
![[2190-4286-16-42-8]](/bjnano/content/figures/2190-4286-16-42-8.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 8: DPV measurement of the BSA/mAbs/4-ATP/AuNFs/CSPE recorded in 0.1 M KCl containing 5 mM [Fe(CN)6]3−/4−.
Figure 8: DPV measurement of the BSA/mAbs/4-ATP/AuNFs/CSPE recorded in 0.1 M KCl containing 5 mM [Fe(CN)6]3−/...
Different antigens of the influenza A H1N1 virus have been targeted for detection over the years. In order to make a substantial comparison, reported systems that targeted the H1 antigen are compared to our system in Table 1. The biosensing system developed in this work shows an acceptable LOD and can be included among biosensors for rapid detection (within minutes) of the H1 protein. In addition, the biosensing system of this work is also compared to other biosensors that employ the DPV technique to target either the hemagglutinin protein or the entire influenza A H1N1 virus. It is observed that the DPV technique offers acceptable LOD and rapid detection times, which are desirable features in biosensing systems.
Table 1: Comparison of the designed electrochemical biosensor to other systems from the literature that target influenza A H1N1 virus.
| Biosensor detection technique | Analyte | Time to detection | LOD | Reference |
| colorimetry | hemagglutinin | 12 h | 11 pg/mL | [13] |
| DPV | hemagglutinin | 1 min | 9 pM (540 pg/mL)a | [14] |
| field-effect transistor | hemagglutinin | 10 min | 0.03 pg/mL | [18] |
| LSPRb | hemagglutinin | — | 1 pM (60 pg/mL)a | [20] |
| ELISA | hemagglutinin | 4 h | — | [47] |
| square wave voltammetry | whole virus | 30 min | 1.52 PFU/mL | [48] |
| DPV | hemagglutinin | 30 min | 3.7 PFU/mL | [49] |
| DPV | whole virus | 30 min | 0.76 pg/mL | [50] |
| DPV | whole virus | 12 h | 0.25 pg/mL | [51] |
| DPV | whole virus | 10 min | 100 ng/mL | [52] |
| DPV | hemagglutinin | 25 min | 19 pg/mL | this work |
aThe molecular weight of H1 is 60 kDa [53]; bLSPR = local surface plasmon resonance.
The biosensor developed in this study can be manufactured with antibodies targeting pandemic influenza strains such as the latest H1N1 that emerged in 2009, also known as the Swine Flu. Since then, H1N1 has been circulating in the community together with other seasonal influenza strains, and surveillance of this virus is required [54]. Furthermore, because of the potential advantage of changing specific monoclonal antibodies in the system, it can easily be adjusted for any and multiple seasonal influenza strains, similar to the case of annual influenza vaccines, which are updated every year to match the currently circulating viruses [55]. Additionally, this characteristic could allow our biosensing platform to be used in mass testing in a short period of time, which is crucial for controlling the spread of a virus among the population. This biosensing platform has the potential to be adapted to target other respiratory viruses such as SARS-CoV-2, a virus for which it has been shown that it can be detected in saliva samples [55].
Our biosensing system for the detection of hemagglutinin protein of influenza A H1N1 virus is currently limited to solutions of the H1 protein in artificial saliva. Future validation tests with clinical samples containing intact virus particles will reveal the potential of this biosensor to be applied for the rapid detection of the influenza A virus. We believe that the use of clinical samples will enable increased sensitivity due to the size and weight of the intact virus (as compared to the H1 protein itself), as well as due to the presence of large number of H1 molecules on the surface of the viral particles.
Conclusion
In this study, a label-free biosensing tool for the detection of hemagglutinin protein of the H1N1 influenza A virus was developed. We have modified low-cost carbon screen-printed electrodes with gold nanoflowers via electrodeposition, functionalized the gold nanoflowers with 4-aminothiophenol, immobilized monoclonal antibodies that specifically target H1 protein, and used BSA to prevent non-specific binding. Differential pulse voltammetry was used in the electrochemical detection of H1 in artificial saliva revealing that the biosensor performs with good reproducibility and sensitivity in the clinically relevant concentration range. The LOD for hemagglutinin is 19 pg/mL, and a good correlation between hemagglutinin concentration and peak current was observed in the concentration range from 10 to 10 000 pg/mL. The experimental EIS data suggest that the electron transfer on the electrode was enhanced by a factor of 100 due to the increase in surface area and to a tunneling charge transfer effect. This improvement is attributed to the synergistic effect of the electrodeposited gold nanoflowers and the functionalization with 4-aminothiophenol. Furthermore, the developed biosensor can be attached to a 3D-printed microfluidic system to be used as a point-of-care device without any significant deleterious effect on the electrochemical performance of the biosensor.
Experimental
Reagents and Materials
Carbon screen-printed electrodes (CSPEs) were obtained from Zimmer & Peacock (Norway). Hemagglutinin protein of influenza A H1N1 virus (H1) and mouse monoclonal antibodies (mAbs) were purchased from Sinobiological (Germany). Secondary goat anti-rabbit IgG antibodies Alexa Flour 568 were obtained from ThermoFisher (USA). Artificial saliva was obtained from LCTech GmbH (Germany). Syringeless filters of regenerated cellulose membrane (0.45 μm) were purchased from Cytiva (Sweden). Chloroauric acid (HAuCl4), hydrochloric acid, sulfuric acid, 4-aminothiophenol (4-ATP), ethanol, potassium chloride, potassium hexacyanoferrate(II) trihydrate, potassium hexacyanoferrate(III), N-(3-dimethylaminopropyl)-N′-ethylcarbodiimide hydrochloride (EDC), N-hydroxy succinimide (NHS), phosphate-buffered saline pH 7.4 (PBS), and bovine serum albumin (BSA) were all purchased from Sigma-Aldrich (Germany) and were used without further purification.
Electrodeposition of gold nanoflowers
The electrodeposition of AuNFs was carried out to increase the surface area of the electrodes. The AuNFs were synthesized following a method from the literature [56] with some modifications. Briefly, 50 μL of a 2 mM HAuCl4 solution containing 6 mM HCl and 0.5 M sulfuric acid was added on top of the CSPE, and a potential of −0.25 V (vs Ag/AgCl) was applied for 60 s. The electrode was then rinsed with 25 mL deionized water, dried under a flow of N2, and stored at room temperature (RT) in dark.
Functionalization with 4-ATP
The surface of the electrodes was functionalized to introduce an amine group, which was used to covalently bind the mAbs as biorecognition element. The molecule 4-ATP possesses a thiol group capable of self-assembling on the surface of the AuNFs. A method from the literature [57] with some modifications was employed. Briefly, the working electrode was covered with 10 μL of 10 mM 4-ATP solution in ethanol and incubated at 22 °C for 15 min. Unreacted 4-ATP was removed by two consecutive washings with 1 mL of ethanol and 1 mL of PBS, respectively. The 4-ATP/AuNFs/CSPE electrode was then dried under a flow of N2 gas and stored at 4 °C until use.
Immobilization of mAbs
The mAbs are essential in our biosensor and function as biorecognition element toward H1 protein. The mAbs were immobilized as described previously [58] with some modifications. Briefly, a reaction mixture of 300 μL was prepared in a 1.5 mL Eppendorf vial by adding 100 μL of 38 μg/mL mABs solution in PBS, 100 μL of 10 mM EDC aqueous solution, and 100 μL of 10 mM NHS aqueous solution. The pH of the mixture was 6.5 as determined by litmus paper. Then, 10 μL of the mixture was added on top of the 4-ATP/AuNFs/CSPE as working electrode and incubated at 4 °C overnight. Afterwards, the mAb/4-ATP/AuNFs/CSPE was rinsed with 1 mL of PBS to remove unreacted species and dried under a flow of N2 gas. The surface of the electrode was blocked by adding 10 μL of 0.5% BSA solution in PBS and incubated at 4 °C for 2 h. Thereafter, the BSA/mAb/4-ATP/AuNFs/CSPE was rinsed with 1 mL of PBS, dried under a flow of N2, and stored at 4 °C.
Quantification of hemagglutinin
A serial dilution of H1 from 10 to 10,000 pg/mL spiked in artificial saliva were prepared from a 100 μg/mL stock solution in PBS. A solution of artificial saliva with no hemagglutinin was used as negative control. After filtrating the solutions through a 0.45 μm membrane filter to remove any suspended particles, 50 μL were deposited on the functionalized electrode and incubated at RT for 25 min. The electrode was then rinsed with 1 mL of PBS and dried under a flow of N2 gas. Subsequently, 50 μL of a 5 mM [Fe(CN)6]3−/4− in 0.1 M KCl solution were used to cover the electrode, and a DPV experiment was performed to characterize the surface of the electrode.
The obtained voltammograms were used to generate a calibration curve, in which the change in current is proportional to the logarithm of the concentration of H1 in the solution. The limit of detection (LOD) was calculated following a conventional criterion where LOD is equal to the mean of the signal of a blank solution plus three standard deviations [39]. The mean of the signal was obtained from a series of DPV experiments after exposing the biosensor to blank solutions of artificial saliva without H1 protein.
Electrochemical measurements
The commercial CSPE employed in this study consists of a three-electrode cell array with a carbon working electrode, a Ag/AgCl reference electrode, and a carbon counter electrode. Potentiostat EmStat Pico with PSTrace 5.8 software was employed to carry out CV, EIS, and DPV experiments. All the experiments were performed in the presence of 5 mM [Fe(CN)6]3−/4− in 0.1 M KCl solution. EIS measurements were performed applying a 6 mV potential at different frequencies from 5 mHz to 50 kHz. DPV measurements were performed with equilibration of 5 s, scanning potential from 0.3 to −0.3 V (vs Ag/AgCl), Estep = 0.01 V, Epulse = 0.086 V, and tpulse = 4 s at a scan rate of 100 mV/s.
SEM analysis of AuNFs
Prior to SEM imaging, the electrode samples were sputtered with a layer of gold/palladium for 40 s at 2 kV (Emitech SC7640, Quorum technologies). Representative micrographs of the AuNFs were taken using a secondary in-lens detector at a working distance of 1.6 mm and an acceleration voltage of 10 keV (Ziess LEO 1530, AB Carl Zeiss). The size distribution of the AuNFs was calculated by measuring the AuNFs in the micrograph presented in Figure 2c, a total of 540 AuNFs were identified and measured with the open-source ImageJ software [59].
Microfluidics system
A microfluidics device (Figure 9) was designed to use the biosensor in point-of-care applications. This system was coupled to a peristaltic pump, and it allowed us to automate the addition of the sample and the reagents to the electrodes during the quantification of hemagglutinin. The microfluidic device, which was printed using a 3D printer (Ultimaker 2+, Ultimaker), contained a slot through which the electrode can be placed and sealed in place using silicon glue (Elastosil A07, Wacker). The device also consisted of two inlets and one outlet through which reagents can be made to pass through the device. The inlets and outlets were connected to reagent sources using silicon tubing (inner diameter = 1 mm, VWR).
![[2190-4286-16-42-9]](/bjnano/content/figures/2190-4286-16-42-9.png?scale=2.0&max-width=1024&background=FFFFFF)
Figure 9: Microfluidics design for point-of-care applications, the dimensions are in millimeters, and a photograph of the entire device is shown.
Figure 9: Microfluidics design for point-of-care applications, the dimensions are in millimeters, and a photo...
Supporting Information
| Supporting Information File 1: Additional experimental details, electrode stability in different solvents, and circuit fitting for the EIS data. | ||
| Format: PDF | Size: 443.0 KB | Download |
Data Availability Statement
All data that supports the findings of this study is available in the published article and/or the supporting information of this article.
References
-
Liu, Q.; Zhou, Y.-h.; Yang, Z.-q. Cell. Mol. Immunol. 2016, 13, 3–10. doi:10.1038/cmi.2015.74
Return to citation in text: [1] -
Webster, R. G.; Govorkova, E. A. Ann. N. Y. Acad. Sci. 2014, 1323, 115–139. doi:10.1111/nyas.12462
Return to citation in text: [1] -
Ravina; Dalal, A.; Mohan, H.; Prasad, M.; Pundir, C. S. Biosci. Rep. 2020, 40, BSR20193852. doi:10.1042/bsr20193852
Return to citation in text: [1] -
Chen, J.-R.; Ma, C.; Wong, C.-H. Trends Biotechnol. 2011, 29, 426–434. doi:10.1016/j.tibtech.2011.04.007
Return to citation in text: [1] -
Zhang, N.; Wang, L.; Deng, X.; Liang, R.; Su, M.; He, C.; Hu, L.; Su, Y.; Ren, J.; Yu, F.; Du, L.; Jiang, S. J. Med. Virol. 2020, 92, 408–417. doi:10.1002/jmv.25674
Return to citation in text: [1] [2] -
Yuan, Q.; Cheng, X.-D.; Yang, B.-C.; Zheng, Q.-B.; Chen, Y.-X.; Chen, Q.-R.; Zeng, F.; Zhang, R.; Ge, S.-X.; Hao, X.-K.; Chen, H.; Zhang, J.; Xia, N.-S. Clin. Microbiol. Infect. 2011, 17, 1574–1580. doi:10.1111/j.1469-0691.2010.03413.x
Return to citation in text: [1] -
Bhalla, N.; Jolly, P.; Formisano, N.; Estrela, P. Essays Biochem. 2016, 60, 1–8. doi:10.1042/ebc20150001
Return to citation in text: [1] -
Anik, Ü.; Tepeli, Y.; Diouani, M. F. Anal. Chem. (Washington, DC, U. S.) 2016, 88, 6151–6153. doi:10.1021/acs.analchem.6b01720
Return to citation in text: [1] [2] -
Joshi, S. R.; Sharma, A.; Kim, G.-H.; Jang, J. Mater. Sci. Eng., C 2020, 108, 110465. doi:10.1016/j.msec.2019.110465
Return to citation in text: [1] -
Bhardwaj, J.; Sharma, A.; Jang, J. Biosens. Bioelectron. 2019, 126, 36–43. doi:10.1016/j.bios.2018.10.008
Return to citation in text: [1] -
Singh, R.; Hong, S.; Jang, J. Sci. Rep. 2017, 7, 42771. doi:10.1038/srep42771
Return to citation in text: [1] -
Devarakonda, S.; Singh, R.; Bhardwaj, J.; Jang, J. Sensors 2017, 17, 2597. doi:10.3390/s17112597
Return to citation in text: [1] -
Ahmed, S. R.; Kim, J.; Suzuki, T.; Lee, J.; Park, E. Y. Biotechnol. Bioeng. 2016, 113, 2298–2303. doi:10.1002/bit.25982
Return to citation in text: [1] [2] -
Veerapandian, M.; Hunter, R.; Neethirajan, S. Talanta 2016, 155, 250–257. doi:10.1016/j.talanta.2016.04.047
Return to citation in text: [1] [2] -
Song, S.; Ha, K.; Guk, K.; Hwang, S.-G.; Choi, J. M.; Kang, T.; Bae, P.; Jung, J.; Lim, E.-K. RSC Adv. 2016, 6, 48566–48570. doi:10.1039/c6ra06689e
Return to citation in text: [1] -
Lee, W. S.; Ahn, J.; Jung, S.; Lee, J.; Kang, T.; Jeong, J. BioChip J. 2021, 15, 260–267. doi:10.1007/s13206-021-00027-y
Return to citation in text: [1] -
Park, G.; Kim, H.-O.; Lim, J.-W.; Park, C.; Yeom, M.; Song, D.; Haam, S. Nano Res. 2022, 15, 2254–2262. doi:10.1007/s12274-021-3772-6
Return to citation in text: [1] -
Hideshima, S.; Hinou, H.; Ebihara, D.; Sato, R.; Kuroiwa, S.; Nakanishi, T.; Nishimura, S.-I.; Osaka, T. Anal. Chem. (Washington, DC, U. S.) 2013, 85, 5641–5644. doi:10.1021/ac401085c
Return to citation in text: [1] [2] -
Bhardwaj, J.; Chaudhary, N.; Kim, H.; Jang, J. Anal. Chim. Acta 2019, 1064, 94–103. doi:10.1016/j.aca.2019.03.005
Return to citation in text: [1] -
Lee, T.; Kim, G. H.; Kim, S. M.; Hong, K.; Kim, Y.; Park, C.; Sohn, H.; Min, J. Colloids Surf., B 2019, 182, 110341. doi:10.1016/j.colsurfb.2019.06.070
Return to citation in text: [1] [2] -
Eom, G.; Hwang, A.; Kim, H.; Yang, S.; Lee, D. K.; Song, S.; Ha, K.; Jeong, J.; Jung, J.; Lim, E.-K.; Kang, T. ACS Sens. 2019, 4, 2282–2287. doi:10.1021/acssensors.9b00697
Return to citation in text: [1] -
Takemura, K.; Adegoke, O.; Takahashi, N.; Kato, T.; Li, T.-C.; Kitamoto, N.; Tanaka, T.; Suzuki, T.; Park, E. Y. Biosens. Bioelectron. 2017, 89, 998–1005. doi:10.1016/j.bios.2016.10.045
Return to citation in text: [1] -
Yoo, H.; Shin, J.; Sim, J.; Cho, H.; Hong, S. Biosens. Bioelectron. 2020, 168, 112561. doi:10.1016/j.bios.2020.112561
Return to citation in text: [1] -
Wu, K.; Liu, J.; Saha, R.; Su, D.; Krishna, V. D.; Cheeran, M. C.-J.; Wang, J.-P. ACS Appl. Mater. Interfaces 2020, 12, 13686–13697. doi:10.1021/acsami.0c00815
Return to citation in text: [1] -
Karn-orachai, K.; Sakamoto, K.; Laocharoensuk, R.; Bamrungsap, S.; Songsivilai, S.; Dharakul, T.; Miki, K. RSC Adv. 2016, 6, 97791–97799. doi:10.1039/c6ra17143e
Return to citation in text: [1] -
Lei, K. F.; Huang, C.-H.; Kuo, R.-L.; Chang, C.-K.; Chen, K.-F.; Tsao, K.-C.; Tsang, N.-M. Anal. Chim. Acta 2015, 883, 37–44. doi:10.1016/j.aca.2015.02.071
Return to citation in text: [1] -
Ma, Y.-D.; Chen, Y.-S.; Lee, G.-B. Sens. Actuators, B 2019, 296, 126647. doi:10.1016/j.snb.2019.126647
Return to citation in text: [1] -
Zhu, Y.; Gu, X.; Tang, Q.; Jiang, W.; Xia, R.; Zhang, J.; Ji, H.; Qin, Y.; Wu, L. Anal. Chem. (Washington, DC, U. S.) 2024, 96, 14116–14124. doi:10.1021/acs.analchem.4c01570
Return to citation in text: [1] -
Tian, Y.; Zhang, Y.; Lu, X.; Xiao, D.; Zhou, C. Anal. Biochem. 2024, 693, 115583. doi:10.1016/j.ab.2024.115583
Return to citation in text: [1] -
Siuzdak, K.; Niedziałkowski, P.; Sobaszek, M.; Łęga, T.; Sawczak, M.; Czaczyk, E.; Dziąbowska, K.; Ossowski, T.; Nidzworski, D.; Bogdanowicz, R. Sens. Actuators, B 2019, 280, 263–271. doi:10.1016/j.snb.2018.10.005
Return to citation in text: [1] -
Jain, R.; Nirbhaya, V.; Chandra, R.; Kumar, S. Electroanalysis 2022, 34, 43–55. doi:10.1002/elan.202100242
Return to citation in text: [1] -
Ezzati, M.; Shahrokhian, S.; Hosseini, H. ACS Sustainable Chem. Eng. 2020, 8, 14340–14352. doi:10.1021/acssuschemeng.0c03806
Return to citation in text: [1] -
Elgrishi, N.; Rountree, K. J.; McCarthy, B. D.; Rountree, E. S.; Eisenhart, T. T.; Dempsey, J. L. J. Chem. Educ. 2018, 95, 197–206. doi:10.1021/acs.jchemed.7b00361
Return to citation in text: [1] -
Fanjul-Bolado, P.; Hernández-Santos, D.; Lamas-Ardisana, P. J.; Martín-Pernía, A.; Costa-García, A. Electrochim. Acta 2008, 53, 3635–3642. doi:10.1016/j.electacta.2007.12.044
Return to citation in text: [1] [2] -
Wongkaew, N.; Simsek, M.; Griesche, C.; Baeumner, A. J. Chem. Rev. 2019, 119, 120–194. doi:10.1021/acs.chemrev.8b00172
Return to citation in text: [1] -
Hu, X.; Wang, T.; Wang, L.; Dong, S. J. Phys. Chem. C 2007, 111, 6962–6969. doi:10.1021/jp0712194
Return to citation in text: [1] [2] -
Zhou, Q.; Li, X.; Fan, Q.; Zhang, X.; Zheng, J. Angew. Chem. 2006, 118, 4074–4077. doi:10.1002/ange.200504419
Return to citation in text: [1] -
Hassan, M. S.; Basera, P.; Bera, S.; Mittal, M.; Ray, S. K.; Bhattacharya, S.; Sapra, S. ACS Appl. Mater. Interfaces 2020, 12, 7317–7325. doi:10.1021/acsami.9b20050
Return to citation in text: [1] -
Serafín, V.; Torrente-Rodríguez, R. M.; González-Cortés, A.; García de Frutos, P.; Sabaté, M.; Campuzano, S.; Yáñez-Sedeño, P.; Pingarrón, J. M. Talanta 2018, 179, 131–138. doi:10.1016/j.talanta.2017.10.063
Return to citation in text: [1] [2] -
Wang, M.; Wang, L.; Wang, G.; Ji, X.; Bai, Y.; Li, T.; Gong, S.; Li, J. Biosens. Bioelectron. 2004, 19, 575–582. doi:10.1016/s0956-5663(03)00252-5
Return to citation in text: [1] -
Chen, Y.; Liu, X.-M.; Wu, X.; Liu, X.-C.; Dong, W.-H.; Han, B.-K.; Du, X.; Zhang, C.; Zhang, Y.-Y.; Wang, H.-T.; Chen, Q. Electrochim. Acta 2017, 258, 988–997. doi:10.1016/j.electacta.2017.11.150
Return to citation in text: [1] -
Li, G.-j.; Liu, L.-h.; Qi, X.-w.; Guo, Y.-q.; Sun, W.; Li, X.-l. Electrochim. Acta 2012, 63, 312–317. doi:10.1016/j.electacta.2011.12.107
Return to citation in text: [1] -
Wu, T.; Wei, X.; Ma, X.; Li, J. Microchim. Acta 2017, 184, 2901–2907. doi:10.1007/s00604-017-2281-5
Return to citation in text: [1] -
Vashist, S. K.; Lam, E.; Hrapovic, S.; Male, K. B.; Luong, J. H. T. Chem. Rev. 2014, 114, 11083–11130. doi:10.1021/cr5000943
Return to citation in text: [1] -
Palomar, Q.; Xu, X.; Gondran, C.; Holzinger, M.; Cosnier, S.; Zhang, Z. Microchim. Acta 2020, 187, 363. doi:10.1007/s00604-020-04339-y
Return to citation in text: [1] -
Rodríguez-Lorenzo, L.; Garrido-Maestu, A.; Bhunia, A. K.; Espiña, B.; Prado, M.; Diéguez, L.; Abalde-Cela, S. ACS Appl. Nano Mater. 2019, 2, 6081–6086. doi:10.1021/acsanm.9b01223
Return to citation in text: [1] -
Lu, C.-Y.; Chang, L.-Y.; Chen, P.-J.; Xia, N.-S.; Shao, P.-L.; Huang, L.-M. J. Formosan Med. Assoc. 2012, 111, 693–697. doi:10.1016/j.jfma.2011.11.029
Return to citation in text: [1] -
Kim, J. H.; Shin, J. H.; Cho, C. H.; Hwang, J.; Kweon, D.-H.; Park, T. J.; Choi, C.-H.; Park, J. P. Talanta 2022, 248, 123613. doi:10.1016/j.talanta.2022.123613
Return to citation in text: [1] -
Bhardwaj, J.; Chaudhary, N.; Kim, H.; Jang, J. Anal. Chim. Acta 2019, 1064, 94–103. doi:10.1016/j.aca.2019.03.005
Return to citation in text: [1] -
Yang, Z.-H.; Zhuo, Y.; Yuan, R.; Chai, Y.-Q. Biosens. Bioelectron. 2016, 78, 321–327. doi:10.1016/j.bios.2015.10.073
Return to citation in text: [1] -
Bao, Q.; Li, G.; Yang, Z.; Liu, J.; Wang, H.; Pang, G.; Guo, Q.; Wei, J.; Cheng, W.; Lin, L. Ionics 2023, 29, 2021–2029. doi:10.1007/s11581-023-04944-w
Return to citation in text: [1] -
Ravina; Gill, P. S.; Narang, J.; Kumar, A.; Mohan, H. 3 Biotech 2022, 12, 141. doi:10.1007/s13205-022-03200-8
Return to citation in text: [1] -
Sriwilaijaroen, N.; Suzuki, Y. Proc. Jpn. Acad., Ser. B 2012, 88, 226–249. doi:10.2183/pjab.88.226
Return to citation in text: [1] -
Khanna, M.; Kumar, B.; Gupta, A.; Kumar, P. Indian J. Virol. 2012, 23, 12–17. doi:10.1007/s13337-012-0066-3
Return to citation in text: [1] -
Cañete, M. G.; Valenzuela, I. M.; Garcés, P. C.; Massó, I. C.; González, M. J.; Providell, S. G. Oral Surg., Oral Med., Oral Pathol., Oral Radiol. 2021, 131, 540–548. doi:10.1016/j.oooo.2021.01.028
Return to citation in text: [1] [2] -
Wang, Y.-C.; Cokeliler, D.; Gunasekaran, S. Electroanalysis 2015, 27, 2527–2536. doi:10.1002/elan.201500120
Return to citation in text: [1] -
Valério, E.; Abrantes, L. M.; Viana, A. S. Electroanalysis 2008, 20, 2467–2474. doi:10.1002/elan.200804350
Return to citation in text: [1] -
Rezki, M.; Septiani, N. L. W.; Iqbal, M.; Harimurti, S.; Sambegoro, P.; Adhika, D. R.; Yuliarto, B. J. Mater. Chem. B 2021, 9, 5711–5721. doi:10.1039/d1tb00222h
Return to citation in text: [1] -
Schneider, C. A.; Rasband, W. S.; Eliceiri, K. W. Nat. Methods 2012, 9, 671–675. doi:10.1038/nmeth.2089
Return to citation in text: [1]
| 45. | Palomar, Q.; Xu, X.; Gondran, C.; Holzinger, M.; Cosnier, S.; Zhang, Z. Microchim. Acta 2020, 187, 363. doi:10.1007/s00604-020-04339-y |
| 46. | Rodríguez-Lorenzo, L.; Garrido-Maestu, A.; Bhunia, A. K.; Espiña, B.; Prado, M.; Diéguez, L.; Abalde-Cela, S. ACS Appl. Nano Mater. 2019, 2, 6081–6086. doi:10.1021/acsanm.9b01223 |
| 13. | Ahmed, S. R.; Kim, J.; Suzuki, T.; Lee, J.; Park, E. Y. Biotechnol. Bioeng. 2016, 113, 2298–2303. doi:10.1002/bit.25982 |
| 1. | Liu, Q.; Zhou, Y.-h.; Yang, Z.-q. Cell. Mol. Immunol. 2016, 13, 3–10. doi:10.1038/cmi.2015.74 |
| 5. | Zhang, N.; Wang, L.; Deng, X.; Liang, R.; Su, M.; He, C.; Hu, L.; Su, Y.; Ren, J.; Yu, F.; Du, L.; Jiang, S. J. Med. Virol. 2020, 92, 408–417. doi:10.1002/jmv.25674 |
| 27. | Ma, Y.-D.; Chen, Y.-S.; Lee, G.-B. Sens. Actuators, B 2019, 296, 126647. doi:10.1016/j.snb.2019.126647 |
| 28. | Zhu, Y.; Gu, X.; Tang, Q.; Jiang, W.; Xia, R.; Zhang, J.; Ji, H.; Qin, Y.; Wu, L. Anal. Chem. (Washington, DC, U. S.) 2024, 96, 14116–14124. doi:10.1021/acs.analchem.4c01570 |
| 29. | Tian, Y.; Zhang, Y.; Lu, X.; Xiao, D.; Zhou, C. Anal. Biochem. 2024, 693, 115583. doi:10.1016/j.ab.2024.115583 |
| 50. | Yang, Z.-H.; Zhuo, Y.; Yuan, R.; Chai, Y.-Q. Biosens. Bioelectron. 2016, 78, 321–327. doi:10.1016/j.bios.2015.10.073 |
| 4. | Chen, J.-R.; Ma, C.; Wong, C.-H. Trends Biotechnol. 2011, 29, 426–434. doi:10.1016/j.tibtech.2011.04.007 |
| 30. | Siuzdak, K.; Niedziałkowski, P.; Sobaszek, M.; Łęga, T.; Sawczak, M.; Czaczyk, E.; Dziąbowska, K.; Ossowski, T.; Nidzworski, D.; Bogdanowicz, R. Sens. Actuators, B 2019, 280, 263–271. doi:10.1016/j.snb.2018.10.005 |
| 51. | Bao, Q.; Li, G.; Yang, Z.; Liu, J.; Wang, H.; Pang, G.; Guo, Q.; Wei, J.; Cheng, W.; Lin, L. Ionics 2023, 29, 2021–2029. doi:10.1007/s11581-023-04944-w |
| 3. | Ravina; Dalal, A.; Mohan, H.; Prasad, M.; Pundir, C. S. Biosci. Rep. 2020, 40, BSR20193852. doi:10.1042/bsr20193852 |
| 23. | Yoo, H.; Shin, J.; Sim, J.; Cho, H.; Hong, S. Biosens. Bioelectron. 2020, 168, 112561. doi:10.1016/j.bios.2020.112561 |
| 24. | Wu, K.; Liu, J.; Saha, R.; Su, D.; Krishna, V. D.; Cheeran, M. C.-J.; Wang, J.-P. ACS Appl. Mater. Interfaces 2020, 12, 13686–13697. doi:10.1021/acsami.0c00815 |
| 25. | Karn-orachai, K.; Sakamoto, K.; Laocharoensuk, R.; Bamrungsap, S.; Songsivilai, S.; Dharakul, T.; Miki, K. RSC Adv. 2016, 6, 97791–97799. doi:10.1039/c6ra17143e |
| 48. | Kim, J. H.; Shin, J. H.; Cho, C. H.; Hwang, J.; Kweon, D.-H.; Park, T. J.; Choi, C.-H.; Park, J. P. Talanta 2022, 248, 123613. doi:10.1016/j.talanta.2022.123613 |
| 2. | Webster, R. G.; Govorkova, E. A. Ann. N. Y. Acad. Sci. 2014, 1323, 115–139. doi:10.1111/nyas.12462 |
| 26. | Lei, K. F.; Huang, C.-H.; Kuo, R.-L.; Chang, C.-K.; Chen, K.-F.; Tsao, K.-C.; Tsang, N.-M. Anal. Chim. Acta 2015, 883, 37–44. doi:10.1016/j.aca.2015.02.071 |
| 49. | Bhardwaj, J.; Chaudhary, N.; Kim, H.; Jang, J. Anal. Chim. Acta 2019, 1064, 94–103. doi:10.1016/j.aca.2019.03.005 |
| 8. | Anik, Ü.; Tepeli, Y.; Diouani, M. F. Anal. Chem. (Washington, DC, U. S.) 2016, 88, 6151–6153. doi:10.1021/acs.analchem.6b01720 |
| 8. | Anik, Ü.; Tepeli, Y.; Diouani, M. F. Anal. Chem. (Washington, DC, U. S.) 2016, 88, 6151–6153. doi:10.1021/acs.analchem.6b01720 |
| 21. | Eom, G.; Hwang, A.; Kim, H.; Yang, S.; Lee, D. K.; Song, S.; Ha, K.; Jeong, J.; Jung, J.; Lim, E.-K.; Kang, T. ACS Sens. 2019, 4, 2282–2287. doi:10.1021/acssensors.9b00697 |
| 20. | Lee, T.; Kim, G. H.; Kim, S. M.; Hong, K.; Kim, Y.; Park, C.; Sohn, H.; Min, J. Colloids Surf., B 2019, 182, 110341. doi:10.1016/j.colsurfb.2019.06.070 |
| 7. | Bhalla, N.; Jolly, P.; Formisano, N.; Estrela, P. Essays Biochem. 2016, 60, 1–8. doi:10.1042/ebc20150001 |
| 22. | Takemura, K.; Adegoke, O.; Takahashi, N.; Kato, T.; Li, T.-C.; Kitamoto, N.; Tanaka, T.; Suzuki, T.; Park, E. Y. Biosens. Bioelectron. 2017, 89, 998–1005. doi:10.1016/j.bios.2016.10.045 |
| 47. | Lu, C.-Y.; Chang, L.-Y.; Chen, P.-J.; Xia, N.-S.; Shao, P.-L.; Huang, L.-M. J. Formosan Med. Assoc. 2012, 111, 693–697. doi:10.1016/j.jfma.2011.11.029 |
| 6. | Yuan, Q.; Cheng, X.-D.; Yang, B.-C.; Zheng, Q.-B.; Chen, Y.-X.; Chen, Q.-R.; Zeng, F.; Zhang, R.; Ge, S.-X.; Hao, X.-K.; Chen, H.; Zhang, J.; Xia, N.-S. Clin. Microbiol. Infect. 2011, 17, 1574–1580. doi:10.1111/j.1469-0691.2010.03413.x |
| 14. | Veerapandian, M.; Hunter, R.; Neethirajan, S. Talanta 2016, 155, 250–257. doi:10.1016/j.talanta.2016.04.047 |
| 5. | Zhang, N.; Wang, L.; Deng, X.; Liang, R.; Su, M.; He, C.; Hu, L.; Su, Y.; Ren, J.; Yu, F.; Du, L.; Jiang, S. J. Med. Virol. 2020, 92, 408–417. doi:10.1002/jmv.25674 |
| 9. | Joshi, S. R.; Sharma, A.; Kim, G.-H.; Jang, J. Mater. Sci. Eng., C 2020, 108, 110465. doi:10.1016/j.msec.2019.110465 |
| 10. | Bhardwaj, J.; Sharma, A.; Jang, J. Biosens. Bioelectron. 2019, 126, 36–43. doi:10.1016/j.bios.2018.10.008 |
| 11. | Singh, R.; Hong, S.; Jang, J. Sci. Rep. 2017, 7, 42771. doi:10.1038/srep42771 |
| 12. | Devarakonda, S.; Singh, R.; Bhardwaj, J.; Jang, J. Sensors 2017, 17, 2597. doi:10.3390/s17112597 |
| 13. | Ahmed, S. R.; Kim, J.; Suzuki, T.; Lee, J.; Park, E. Y. Biotechnol. Bioeng. 2016, 113, 2298–2303. doi:10.1002/bit.25982 |
| 14. | Veerapandian, M.; Hunter, R.; Neethirajan, S. Talanta 2016, 155, 250–257. doi:10.1016/j.talanta.2016.04.047 |
| 15. | Song, S.; Ha, K.; Guk, K.; Hwang, S.-G.; Choi, J. M.; Kang, T.; Bae, P.; Jung, J.; Lim, E.-K. RSC Adv. 2016, 6, 48566–48570. doi:10.1039/c6ra06689e |
| 16. | Lee, W. S.; Ahn, J.; Jung, S.; Lee, J.; Kang, T.; Jeong, J. BioChip J. 2021, 15, 260–267. doi:10.1007/s13206-021-00027-y |
| 17. | Park, G.; Kim, H.-O.; Lim, J.-W.; Park, C.; Yeom, M.; Song, D.; Haam, S. Nano Res. 2022, 15, 2254–2262. doi:10.1007/s12274-021-3772-6 |
| 18. | Hideshima, S.; Hinou, H.; Ebihara, D.; Sato, R.; Kuroiwa, S.; Nakanishi, T.; Nishimura, S.-I.; Osaka, T. Anal. Chem. (Washington, DC, U. S.) 2013, 85, 5641–5644. doi:10.1021/ac401085c |
| 19. | Bhardwaj, J.; Chaudhary, N.; Kim, H.; Jang, J. Anal. Chim. Acta 2019, 1064, 94–103. doi:10.1016/j.aca.2019.03.005 |
| 20. | Lee, T.; Kim, G. H.; Kim, S. M.; Hong, K.; Kim, Y.; Park, C.; Sohn, H.; Min, J. Colloids Surf., B 2019, 182, 110341. doi:10.1016/j.colsurfb.2019.06.070 |
| 18. | Hideshima, S.; Hinou, H.; Ebihara, D.; Sato, R.; Kuroiwa, S.; Nakanishi, T.; Nishimura, S.-I.; Osaka, T. Anal. Chem. (Washington, DC, U. S.) 2013, 85, 5641–5644. doi:10.1021/ac401085c |
| 33. | Elgrishi, N.; Rountree, K. J.; McCarthy, B. D.; Rountree, E. S.; Eisenhart, T. T.; Dempsey, J. L. J. Chem. Educ. 2018, 95, 197–206. doi:10.1021/acs.jchemed.7b00361 |
| 31. | Jain, R.; Nirbhaya, V.; Chandra, R.; Kumar, S. Electroanalysis 2022, 34, 43–55. doi:10.1002/elan.202100242 |
| 52. | Ravina; Gill, P. S.; Narang, J.; Kumar, A.; Mohan, H. 3 Biotech 2022, 12, 141. doi:10.1007/s13205-022-03200-8 |
| 32. | Ezzati, M.; Shahrokhian, S.; Hosseini, H. ACS Sustainable Chem. Eng. 2020, 8, 14340–14352. doi:10.1021/acssuschemeng.0c03806 |
| 53. | Sriwilaijaroen, N.; Suzuki, Y. Proc. Jpn. Acad., Ser. B 2012, 88, 226–249. doi:10.2183/pjab.88.226 |
| 54. | Khanna, M.; Kumar, B.; Gupta, A.; Kumar, P. Indian J. Virol. 2012, 23, 12–17. doi:10.1007/s13337-012-0066-3 |
| 39. | Serafín, V.; Torrente-Rodríguez, R. M.; González-Cortés, A.; García de Frutos, P.; Sabaté, M.; Campuzano, S.; Yáñez-Sedeño, P.; Pingarrón, J. M. Talanta 2018, 179, 131–138. doi:10.1016/j.talanta.2017.10.063 |
| 40. | Wang, M.; Wang, L.; Wang, G.; Ji, X.; Bai, Y.; Li, T.; Gong, S.; Li, J. Biosens. Bioelectron. 2004, 19, 575–582. doi:10.1016/s0956-5663(03)00252-5 |
| 41. | Chen, Y.; Liu, X.-M.; Wu, X.; Liu, X.-C.; Dong, W.-H.; Han, B.-K.; Du, X.; Zhang, C.; Zhang, Y.-Y.; Wang, H.-T.; Chen, Q. Electrochim. Acta 2017, 258, 988–997. doi:10.1016/j.electacta.2017.11.150 |
| 42. | Li, G.-j.; Liu, L.-h.; Qi, X.-w.; Guo, Y.-q.; Sun, W.; Li, X.-l. Electrochim. Acta 2012, 63, 312–317. doi:10.1016/j.electacta.2011.12.107 |
| 43. | Wu, T.; Wei, X.; Ma, X.; Li, J. Microchim. Acta 2017, 184, 2901–2907. doi:10.1007/s00604-017-2281-5 |
| 59. | Schneider, C. A.; Rasband, W. S.; Eliceiri, K. W. Nat. Methods 2012, 9, 671–675. doi:10.1038/nmeth.2089 |
| 44. | Vashist, S. K.; Lam, E.; Hrapovic, S.; Male, K. B.; Luong, J. H. T. Chem. Rev. 2014, 114, 11083–11130. doi:10.1021/cr5000943 |
| 38. | Hassan, M. S.; Basera, P.; Bera, S.; Mittal, M.; Ray, S. K.; Bhattacharya, S.; Sapra, S. ACS Appl. Mater. Interfaces 2020, 12, 7317–7325. doi:10.1021/acsami.9b20050 |
| 58. | Rezki, M.; Septiani, N. L. W.; Iqbal, M.; Harimurti, S.; Sambegoro, P.; Adhika, D. R.; Yuliarto, B. J. Mater. Chem. B 2021, 9, 5711–5721. doi:10.1039/d1tb00222h |
| 36. | Hu, X.; Wang, T.; Wang, L.; Dong, S. J. Phys. Chem. C 2007, 111, 6962–6969. doi:10.1021/jp0712194 |
| 39. | Serafín, V.; Torrente-Rodríguez, R. M.; González-Cortés, A.; García de Frutos, P.; Sabaté, M.; Campuzano, S.; Yáñez-Sedeño, P.; Pingarrón, J. M. Talanta 2018, 179, 131–138. doi:10.1016/j.talanta.2017.10.063 |
| 34. | Fanjul-Bolado, P.; Hernández-Santos, D.; Lamas-Ardisana, P. J.; Martín-Pernía, A.; Costa-García, A. Electrochim. Acta 2008, 53, 3635–3642. doi:10.1016/j.electacta.2007.12.044 |
| 56. | Wang, Y.-C.; Cokeliler, D.; Gunasekaran, S. Electroanalysis 2015, 27, 2527–2536. doi:10.1002/elan.201500120 |
| 36. | Hu, X.; Wang, T.; Wang, L.; Dong, S. J. Phys. Chem. C 2007, 111, 6962–6969. doi:10.1021/jp0712194 |
| 37. | Zhou, Q.; Li, X.; Fan, Q.; Zhang, X.; Zheng, J. Angew. Chem. 2006, 118, 4074–4077. doi:10.1002/ange.200504419 |
| 57. | Valério, E.; Abrantes, L. M.; Viana, A. S. Electroanalysis 2008, 20, 2467–2474. doi:10.1002/elan.200804350 |
| 34. | Fanjul-Bolado, P.; Hernández-Santos, D.; Lamas-Ardisana, P. J.; Martín-Pernía, A.; Costa-García, A. Electrochim. Acta 2008, 53, 3635–3642. doi:10.1016/j.electacta.2007.12.044 |
| 55. | Cañete, M. G.; Valenzuela, I. M.; Garcés, P. C.; Massó, I. C.; González, M. J.; Providell, S. G. Oral Surg., Oral Med., Oral Pathol., Oral Radiol. 2021, 131, 540–548. doi:10.1016/j.oooo.2021.01.028 |
| 35. | Wongkaew, N.; Simsek, M.; Griesche, C.; Baeumner, A. J. Chem. Rev. 2019, 119, 120–194. doi:10.1021/acs.chemrev.8b00172 |
| 55. | Cañete, M. G.; Valenzuela, I. M.; Garcés, P. C.; Massó, I. C.; González, M. J.; Providell, S. G. Oral Surg., Oral Med., Oral Pathol., Oral Radiol. 2021, 131, 540–548. doi:10.1016/j.oooo.2021.01.028 |
© 2025 Torres-Méndez et al.; licensee Beilstein-Institut.
This is an open access article licensed under the terms of the Beilstein-Institut Open Access License Agreement (https://www.beilstein-journals.org/bjnano/terms), which is identical to the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0). The reuse of material under this license requires that the author(s), source and license are credited. Third-party material in this article could be subject to other licenses (typically indicated in the credit line), and in this case, users are required to obtain permission from the license holder to reuse the material.